We thought we’d be spending three days in the hospital, but we ended up staying for two weeks. It’s complicated. Here’s what happened.
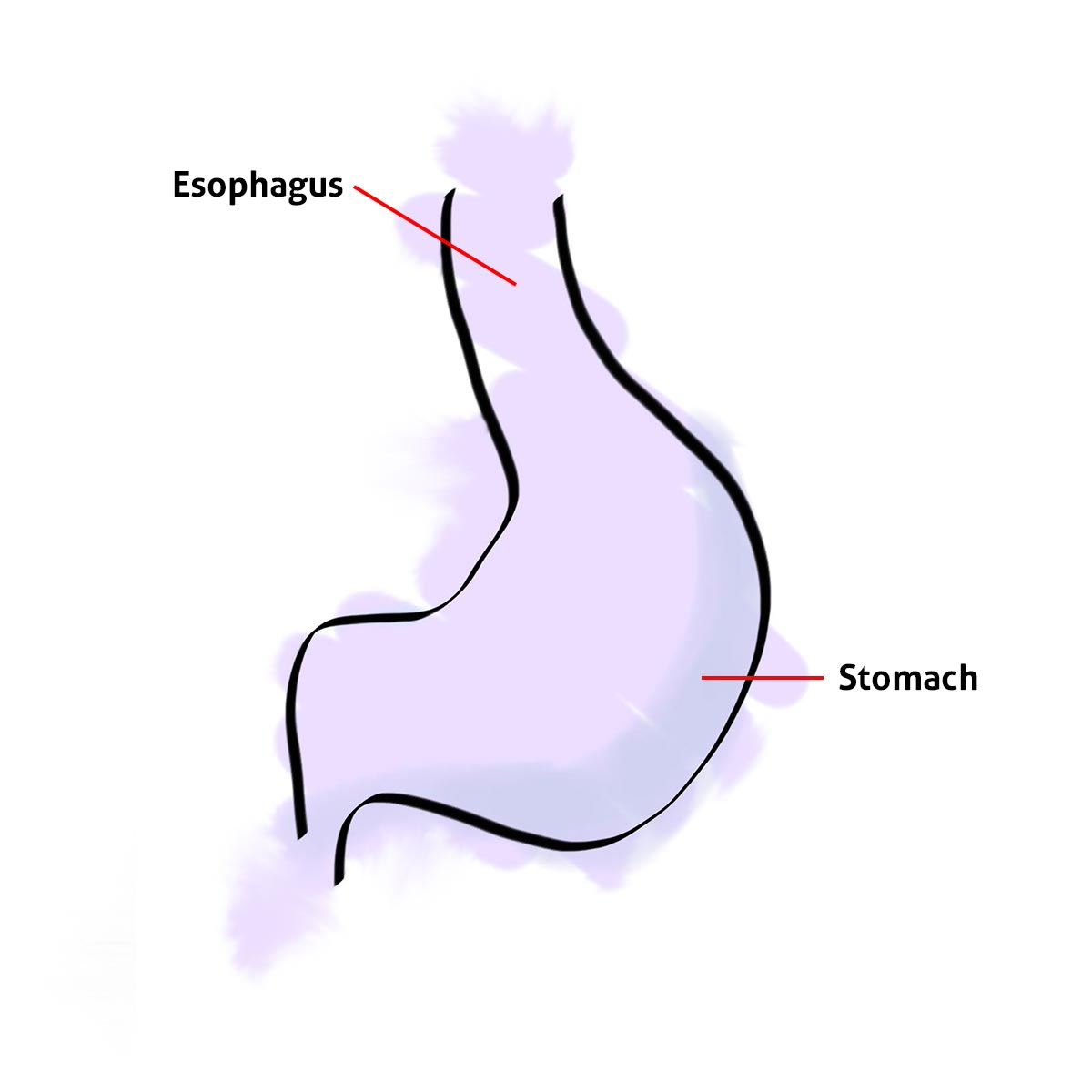
A Typical Baby Stomach
This is sort-of what the stomach of a normal healthy baby looks like. I made these images to illustrate Ayla’s unique stomach, I left out lot’s of detail, but you’ll get the idea.
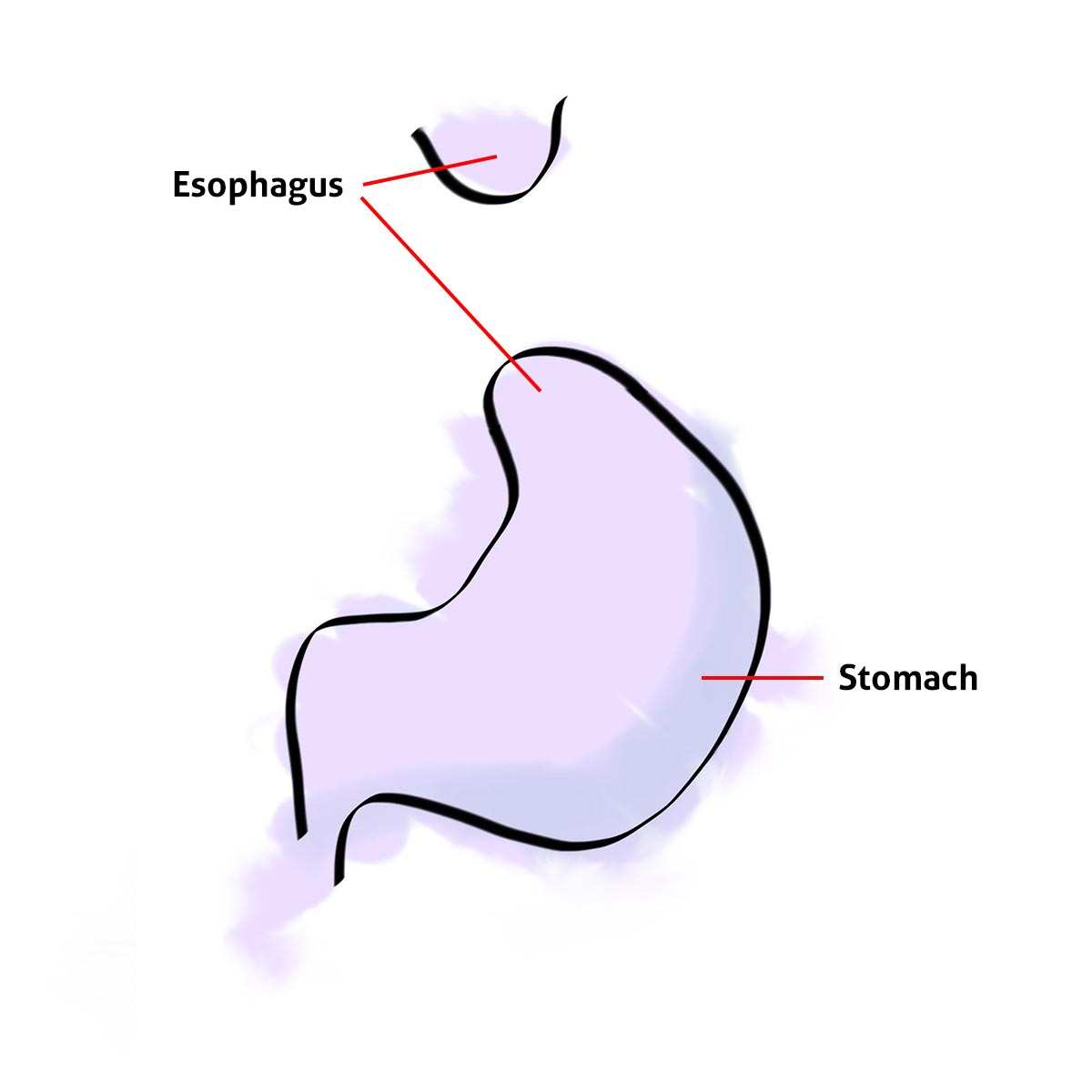
The Stomach Ayla Was Born With
Ayla was born with a TE Fistula. Her esophagus and stomach did not connect and needed to be repaired.
Ayla's Stomach After Her TE Fistula Repair
As you may remember, Ayla’s first surgery happened when she was just three days old. To connect Ayla’s stomach and esophagus, her surgeon, Dr. Saito, had to pull Ayla’s stomach up and esophagus down and join them together. The distance of the separation was substantial and pulling the stomach upward meant the top of the stomach would pass through the diaphragm, creating a Hiatal Hernia.
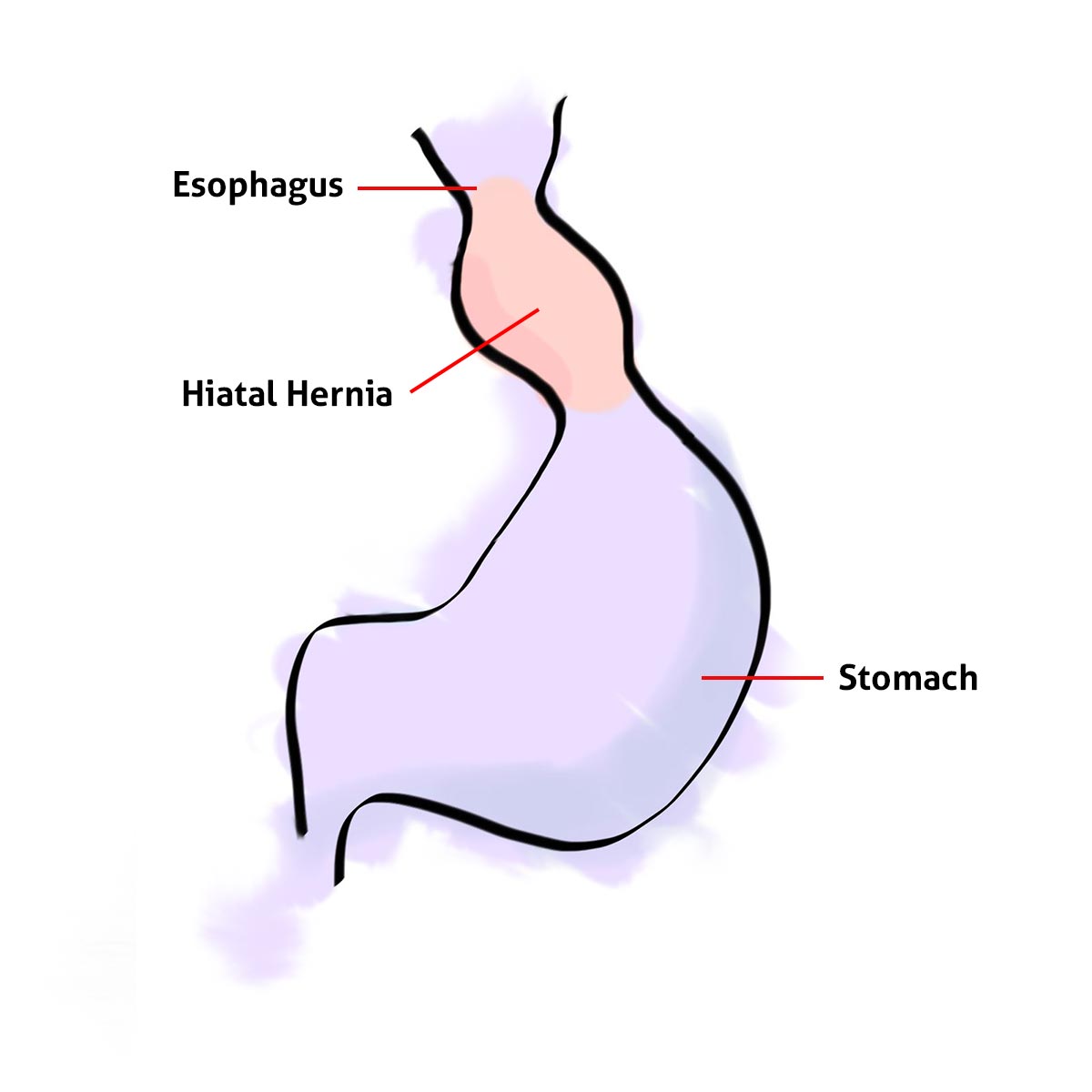
The repair complete, things were going well, but the haital hernia started causing problems. Ayla’s stomach was really tiny since she’d never really had any food/fluid in it. When her stomach filled up, via an NG-Tube, some feeds would make their way up into her haital hernia, and she would reflux. Ayla was spitting up way too much milk/stomach stuff, and because of her micrognathia and limited swallowing function, it was likely that she would damage her TE Fistula repair site, or aspirate, leading to any number of respiratory complications.
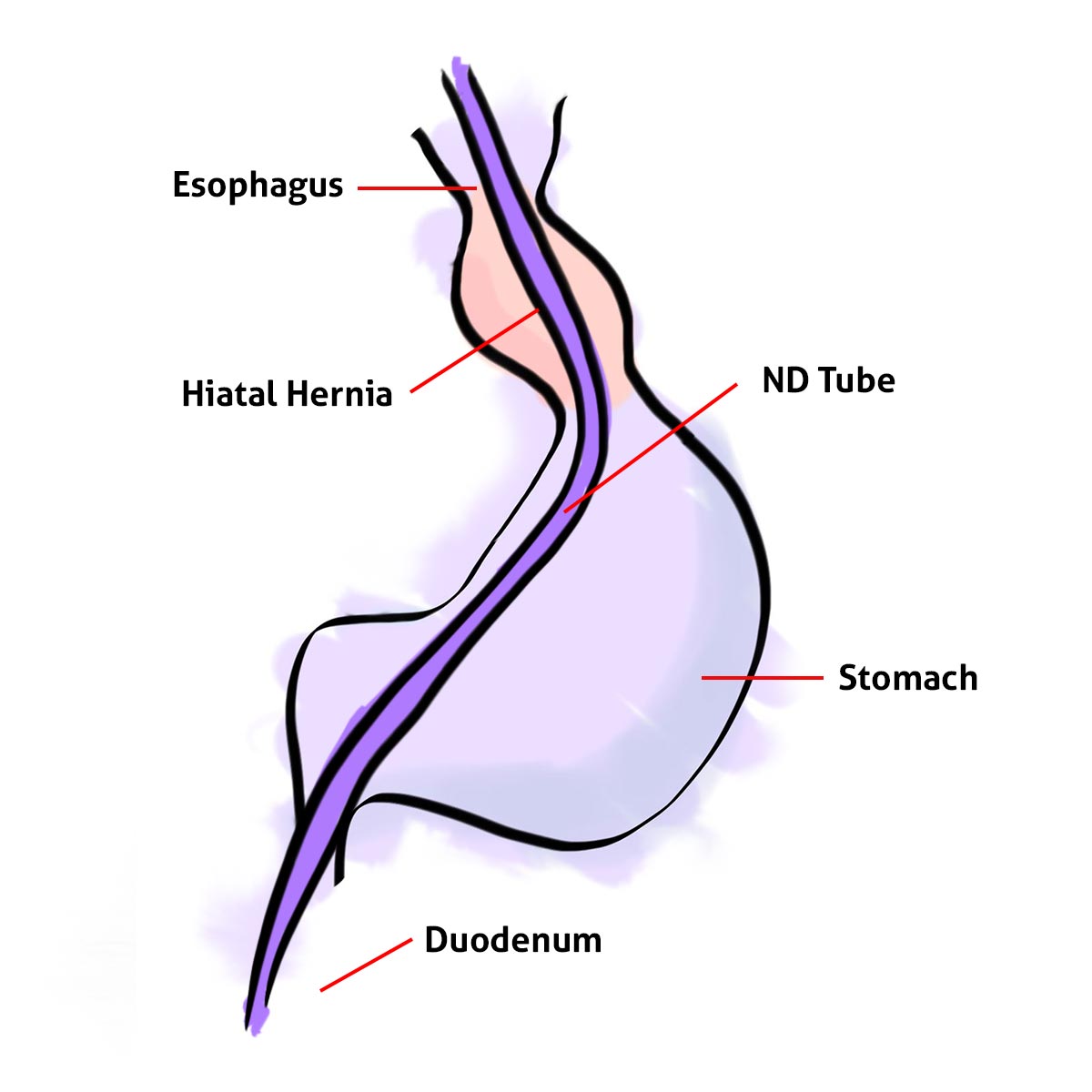
Let's Add an ND-Tube
To solve this problem, the doctors recommended an ND-Tube. The Nasoduodenal (ND) tube is weighted, and was inserted through her nose, into her stomach, and the weights carry it into her Duodenum. This allowed Ayla to receive food, without filling her stomach, and without filling her hiatal hernia. Unfortunately, this also meant that Ayla’s stomach wasn’t going to be stretching and growing. Ok, yes, growing slightly, relative to her size, but it would still be very, very small.
Long-Term Solutions
The ND-Tube was a decent temporary solution, but it meant keeping Ayla on continuous liquid feeds. If we ever wanted to get rid of that tube in her nose, and work up to bolus feeds, she’d need a G-Button. We knew this, but the ND-Tube was going ok, until it started clogging all the time, and Ayla started ripping the tape off of her face and pulling on the tube. It was stressful for us, and painful for Ayla. Especially painful when I had to carefully thread the weighted end of that tube back into her nose.
So we talked to her Surgeon, and we all agreed that she was ready for a G-Button. The surgery would be laparoscopic, requiring just 5 small incisions. One incision would be used for the G-Button itself.
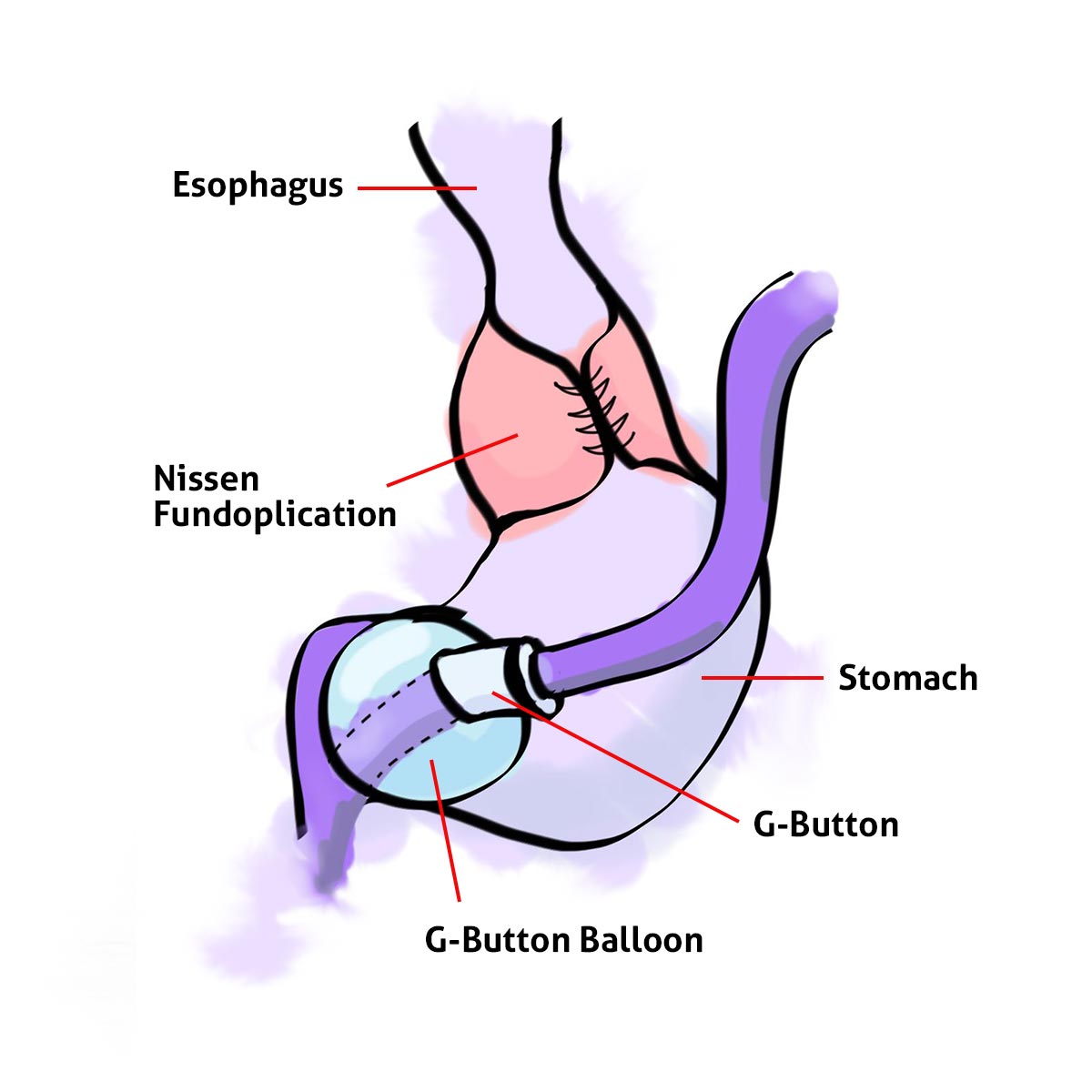
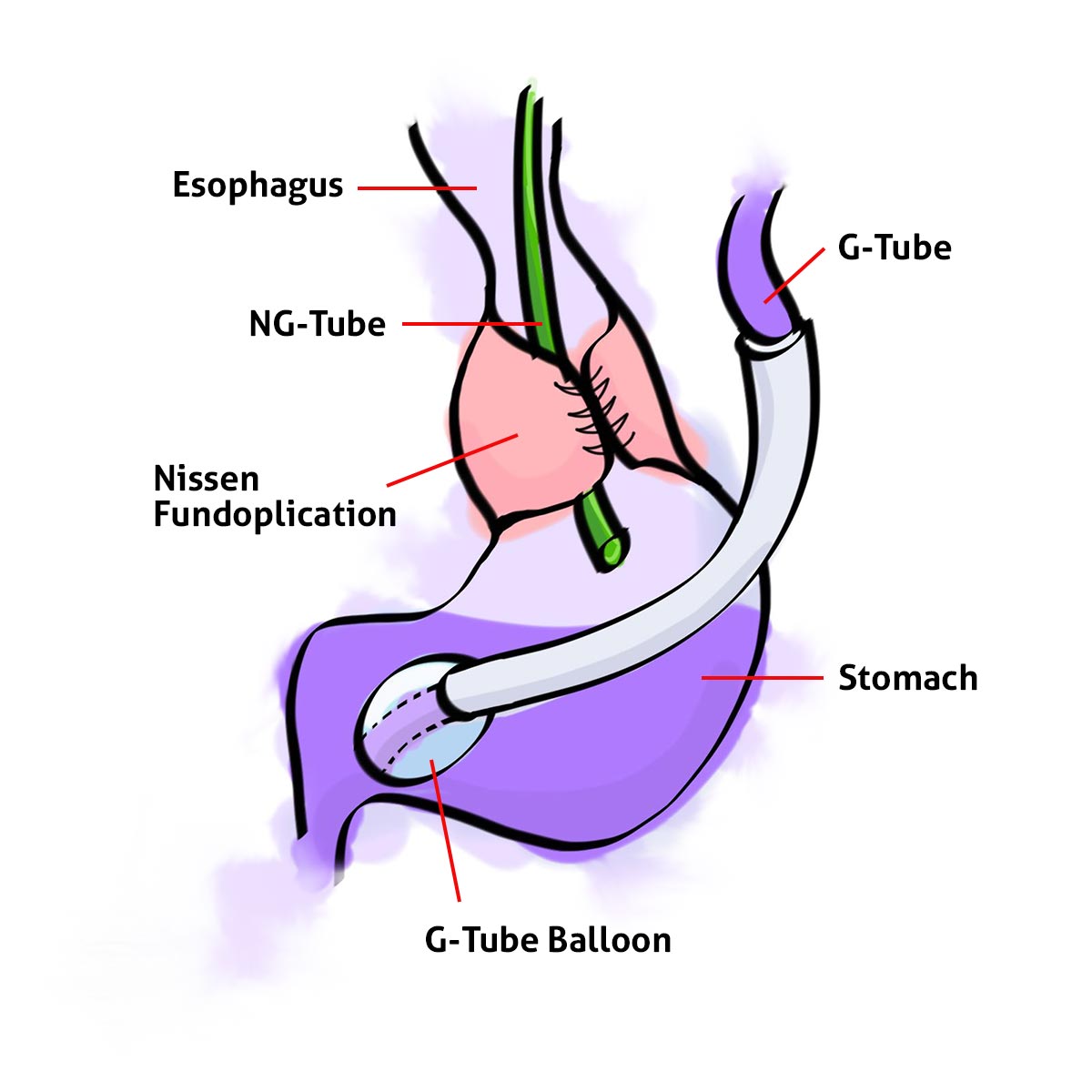
As part of this surgery, Ayla would have her haital hernia repaired, and receive a Nissen Fundoplication. The “Fundo” meant wrapping the top of the stomach around the bottom of the esophagus, creating a one-way valve of sorts, to prevent Ayla from refluxing and potentially damaging her TEF repair site.
PICU - Pulmonary - PICU - Pulmonary
Ayla’s surgery went according to plan. The hernia had been repaired, the Fundo created, and the G-button placed. The NG-Tube was out of her nose and she was recovering. She spent that day and night in the PICU (Pediatric Intensive Care Unit), and was moved to the Pulmonary wing the next afternoon.

We stayed in the room with her that night and managed all of her regular care. She didn’t sleep very well, alarmed a lot, and needed a lot of attention. She wasn’t really herself yet, but we assumed it was just part of her recovery.
On Friday morning Ayla started having some trouble with her oxygen saturations, and she was breathing strangely. We were becoming a bit more concerned. Then she had an episode, with doctors, nurses, and respiratory therapists in the room. It was chaotic for a while. New docs that didn’t really know Ayla were trying to figure her out, Alaina and I are trying to stand back and be patient. Ayla de-sated pretty hard at one point so I stepped in and bagged her. I’m sure the nurse or respiratory therapist would have if I didn’t, but Alaina and I have seen it so much that we know when it’s about to happen so I had already grabbed the bag and was ready to go. She was bagged several times for the next hour or so while the doctors set up the transfer back to the PICU. Ayla was having a hard time and would require closer attention from an ICU nurse. By the evening, she’d settled down. She was doing much better and Alaina and I felt more comfortable now that she was being closely monitored in the PICU, so we left late that night to get some sleep.
Free Air
Before Alaina and I entered Ayla’s room Saturday morning, Alaina said from hall “Somebody’s upset.” I looked up and could also see that Ayla’s heart rate was over 200 bpm and thought “Yep.” We quickly tried to calm her down. Something was off, she didn’t look upset at all. She was breathing really fast and her heart rate was really high, but she seemed happy. We asked the nurse about it, then we asked for a doctor. They thought she was fine and that she’d calm soon. They assumed she was just having a hard time managing her pain. They gave her some morphine and we stood by to see if she would improve. We gave it 5 minutes, then 10 minutes, nothing changed. Inspecting her, we noticed that her stomach was really tight and swollen. They opened her G-Button and tried venting her, but it didn’t help.
I could feel my body language changing, I was growing more impatient by the second. My heart was thumping with a weird mix of chemicals that my body was pouring into my blood to prevent me from losing my mind. In front of me, my baby girl, breathing like she just ran a marathon, her heart racing to dangerously high rates, looks calm, but seems confused by the way she feels and the things that are happening around her. To my left, my wife is on the verge of tears, she’s losing her patience too and she’s asking me what I think is wrong. So we ask the nurses and docs again… please, take action, do something more. Don’t just stand back and watch her heart pound like this. “She’s breathing really hard, maybe something’s up with her trache. I’d like to go ahead and replace it.” The words were barely out of my mouth and they were getting more doctors involved. I think they understood that we’d had enough, and we were going to start troubleshooting.
The Chief of Surgery immediately came in and examined her. He looked at her for all of 30 seconds and then ordered an x-ray of her abdomen. He looked at the x-ray and determined that she had free air throughout her abdomen. He warned that Ayla could have a perforation from the surgery and that she might get very sick, and that she would definitely have Subcutaneous Emphysema. Ayla’s surgeon was called in to the hospital, and they took Ayla in for emergency surgery.
What Went Wrong
Several hours of waiting, and Ayla was finally out of surgery. Her surgeon came out and told us what they’d found.
The G-Button has a balloon on the end of it that they inflate inside of Ayla’s stomach to secure it, preventing it from being pulled out. That little balloon ended up being too big for Ayla’s stomach. It filled the lower part of her stomach, blocking her pyloric sphincter, preventing her stomach from draining and preventing gas from escaping. And because Ayla had just received a fundoplication she couldn’t burp or allow air to escape upward. So air and fluids that did enter Ayla’s stomach were trapped there, until eventually the air pressure was too much and had to escape. Air started escaping around the G-Button hole in her stomach and leaked under her skin, throughout her abdomen.
Fixing It Again
To fix this problem, they had to put in a G-Tube instead of the G-Button. They stitched it in and could leave the balloon inflated only half way so it didn’t fill her stomach and cause the same problem as the g-button. They also placed an NG-Tube which they connected to a repogle allowing Ayla to vent constantly, preventing any air from filling her stomach. The repogle was a temporary solution until we could start venting her from her G-Tube.
After a couple more nights in the PICU, we headed back to the Pulmonary wing again. We spent a few more days there while Ayla recovered and fought off another round of Rhinovirus. I left out some detail and other dramatic moments before and after each surgery, but I hope this give you an idea of what happened.


Thank you, and you, and you
It was a crazy two weeks. To all of you who sent thoughts, prayers, encouragement… thank you. We love you and we needed that. Once again, you came through.
Grandma, thank you for helping throughout that 2 week visit, with everything. We love you.
Mike and Breanne, thank you for coming down to sit in the waiting area with us during Ayla’s emergency surgery. It meant more than we could have expressed right then. We really love you guys.
The comforts of the NICU were dearly missed, but almost ALL of Ayla’s NICU nurses stopped by to visit. We met several new friends in the PICU/Pulmonary floor. The nurses, doctors, and therapists were all terrific. We can’t say enough about the care we’ve received at STL Childrens Hospital. Thank you all so much.
A special thank you to Dr. Saito (Ayla’s Surgeon). We are so thankful for your skill and patience and determination. We feel privileged to have you on Ayla’s team.
Corey, Alaina, and Ayla


It’s amazing to read someone else’s story and feel like I’m reading our own. My son was born with vacterl and he also had complications when they have him his gtube. I fully understand watching the monitors and my husband has stepped in and bagged our son at least once. Thank you for sharing it’s nice to know other people in the world know at least a little how we’ve felt and are making it through. Blessings to you and your wife and sweet little girl.
Thank you for sharing your experience I am so happy that she made it and growing so well. God bless your family.